About Pain Spa
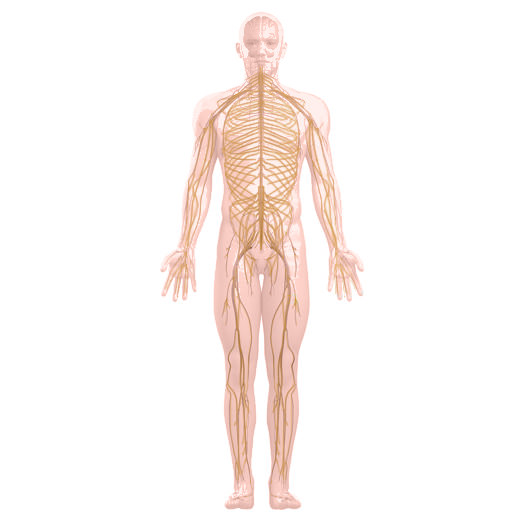
We focus on a holistic approach to pain management, encouraging healthy life style changes and promoting overall well-being.
Find out more
About Pain Spa
We focus on a holistic approach to pain management, encouraging healthy life style changes and promoting overall well-being.